To terminate or not to terminate?
That is the question!
By: Ghada Youssef, MD
A 32-year-old lady, Gravida 2, para 2, with a history of 2 cesarean section deliveries (which were both uneventful), and not a known hypertensive, diabetic or a smoker.
She was presented to the Pregnancy-Heart team at the High-Risk Pregnancy Unit on her 35th week gestation with persistent BP of 160/100 mmHg and sinus tachycardia at a rate 95 bpm. She was diagnosed as HDP (Hypertensive disorder in pregnancy). The patient was admitted to hospital for frequent BP follow up and other investigations were ordered. She was prescribed Labetalol 100 mg bid and Alpha methyl Dopa 250 mg tds and her BP was closely monitored in hospital.
Laboratory findings included: Hb=7 g/dL (hypochromic, microcytic), PLT=85,000/HPF, AST=244 mg/dL, ALT=270 mg/dL, Creatinine=0.9 mg/dL, Albumin=2.4 mg/dL, Proteins in urine= 3 g/24hours, BNP=693 pg/dL.
ECG and fundus examination were normal, and echocardiography showed the following: LVEDD: 5.4 cm, LVESD: 3.3 cm, LVEF: 66%, SWT: 1.1 cm, PWT: 1.0 cm, LA: 3.8 cm and grade 1 diastolic dysfunction.
Based on these investigations, the patient was diagnosed as preeclampsia with severe manifestations and HELLP syndrome.
Obstetric evaluation to the fetus showed absence of signs of maturity.
**In this situation, what would be your decision?
1- Terminate pregnancy immediately.
2- Wait till BP control.
3- Wait for labour pains to begin.
4- Council the patient and wait for 2 more weeks.
As her gestational age was 35 weeks on presentation, the decision was to terminate pregnancy immediately by CS delivery. Her baby was incubated for 2 weeks and was discharged afterwards.
After delivery: her laboratory tests were back to normal after 2 days, her BP dropped to 140/90 mmHg, Alpha methyl Dopa was stopped, and Labetalol dose was reduced to 100 mg qd.
Follow up BP: after 1 month (BP 130/70 mmHg) and Labetalol was discontinued, after 2 months (BP 110/80 mmHg) and after 3 months of delivery BP was 120/70 mmHg.
What do we learn from this case?
– Preeclampsia with severe manifestation is a serious disease that needs hospital admission and close BP and laboratory monitoring.
– Preeclampsia with HELLP syndrome in a pregnant lady with gestational age >34 weeks warrants termination of pregnancy.
– Preeclampsia can recur in a subsequent pregnancy, the incidence is 18%.
– Preeclampsia runs in families, so pregnant ladies with a positive family history of preeclampsia should be closely monitored throughout pregnancy till delivery and after delivery.
– Females with history of preeclampsia have a high incidence of HTN and cardiac diseases later in life, that is why annual assessment of cardiovascular risk is recommended.
Hypertension Case Studies
Mohsen Ibrahim, MD
A female patient with recent severe Hypertension
74 years old female referred because of history of recent severe HT and epistaxis. Two days before her clinic visit while visiting her husband in ICU she stumbled and bled from her nose. BP checked at that time was 220/? mmHg, she was given IV and sublingual medicine and left the hospital with BP 170/90 mmHg though epistaxis continued. On her first clinic visit, epistaxis stopped but she wanted to be reassured regarding her BP. She had no specific complaints except worrying about her husband who had a recent MI and she mentioned that she is under severe stress, and she was in good health before the last event. She was not known to be hypertensive with no history of antihypertensive drug intake or other medication except vitamins and had no family history of HT. she had no history of renal problems, operations, weight changes, intake of pressor medications (NSAIDS). During examination she looked depressed with mild skin pallor, her body weight was 74 kg and height 162cm BP measured supine several times ranged 208/124-180/118 mmHg, heart rate was 128 b/m and regular. Physical examination was unremarkable with intact peripheral pulsations and absence of cardiac or abdominal murmurs. ECG showed sinus tachycardia at a rate of 130 b/m and left atrial abnormality.
Laboratory tests were ordered and the patient was prescribed the following medications and sent home: Bisoprolol 5 mg BID, amlodipine 10 mg.
Valsartan 10 mg combination, torsemide 10 mg, SSRI (faverin 50 mg) and Zolam 0.25 mg.
Next day afternoon, a phone call from her daughter who mentioned that her mother was sleepy all day and her BP was 102/70-104/78 mmHg. She was asked to discontinue faverin and torsemide and to see her after 10 days.
Laboratory tests showed a blood urea of 85mg/dL, creatinine 1.3 mg/dL, uric acid 7.2 mg/dL, K 4.4 mmol/L, HB 11.8 mg/dL with normal blood sugar, TSH and lipid profile.
When patient was seen in her second clinic visit few weeks later, she was symptom free, BP was 164/100 mmHg, her ECG showed frequent PACs, LAE and possible LVH ( R in AVL = 12 mm). treatment was modified to bisoprolol 10 mg, plus a polypill of thiazide / amlodipine/ valsartan 160 mg.
Few weeks later the patient reported through a phone call she is symptom free, her home BP readings 140/80-165/95 mmHg. However her repeat laboratory tests showed a blood urea of 93 mg/dL, creatinine of 1.7 mg/dL while her optic fundus showed atherosclerotic changes and cotton wool exudates.
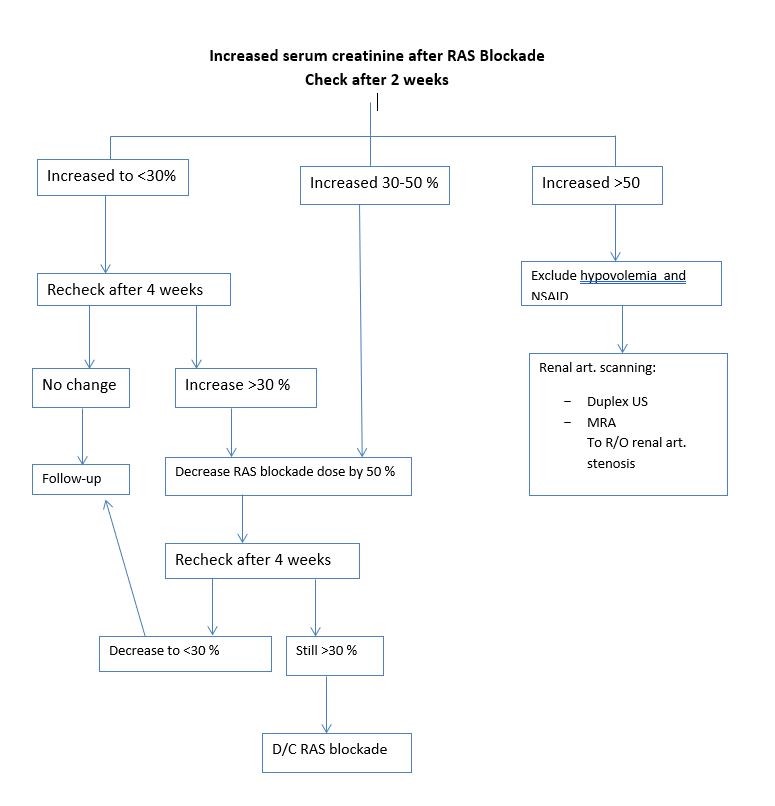
This acute rise in serum creatinine following RAS blockade was alarming. However it is normal up to 30 % of baseline level. However, if there is an increase more than 50% one has to exclude severe hypovolemia, NSAIDs intake, renal artery stenosis, polycystic kidney disease, sepsis or the use of cyclosporine.
On third office visit two months later, patient was symptom free, her home BP readings were 110/70 mmHg, BP at office was 144/90 mmHg, patients was asked to continue same treatment and recheck her serum creatinine and urea which turned out to be elevated . Creatinine was 1.9 mg/dL and urea 106 mg/dL, potassium 4.7 mg/L.
It was decided to discontinue valsartan and to refer the patient for renal artery duplex ultrasound which showed right renal artery stenosis.
Comments:
Clinical findings associated with renal artery stenosis:
Abrupt onset of HT at or after the age of 50 years.
Accelerated or malignant HT.
Refractory HT not responding to therapy with ≥ 3 drugs
Azotemia induced by treatment with RAS blocker.
Unilateral small kidney.
Unexplained hypokalemia
Abdominal bruit or over the flanks.
Severe retinopathy
Unexplained congestive heart failure or acute pulmonary edema
Vascular studies to evaluate the renal arteries:
Duplex ultrasonography: shows renal arteries and measures flow velocity
Magnetic resonance angiography: shows renal arteries and peri renal aorta . It is not nephrotoxic and is useful in patients with renal failure
Computed tomographic- angiography: shows renal arteries and peri renal aorta while providing excellent images. However, the large volume of contrast medium required is potentially nephrotoxic.
Renal artery stenosis
– May occur alone (isolated) or in combination with HT (reno-vascular or essential HT) or renal insufficiency (ischemic nephropathy) or both.
– In patient with renal artery stenosis and HT, HT is seldom cured by revascularization, except in those with fibro muscular dysplasia. Renal revascularization may improve and stabilize renal function in patients with renal artery stenosis and chronic renal failure.
– There is unproven benefit of renal revascularization compared with best medical therapy in atherosclerotic reno vascular disease.