M. Mohsen Ibrahim, MD
Prof. of Cardiology-Cairo University
Address: 1 El-Sherifein St., Abdeen, -Cairo
Tel: (202) 794-8877 / 392-1777
Fax: (202) 794-8879
E-mail: ehs@link.net
The Egyptian Hypertension Society - President Message - M.Mohsen Ibrahim, MD
President Massage (June 2021)
The Making of New Guidelines
Mohsen Ibrahim, MD
President of the Egyptian Hypertension Society
Within the coming weeks the new EHS dyslipidemia guidelines will be available for the medical community. In the following president message I will outline the steps in the preparation of guidelines and the questions addressed when making new guidelines.
- How important is the subject of guidelines?
Coronary heart disease (CHD) is common among Egyptians and possibly its prevalence is on the rise in recent years based upon authors personal practice. Atherosclerotic risk factors namely cigarettes smoking, obesity, hypertension, unhealthy life style and poor dietary habits are common furthermore the number of patients with diabetes mellitus has almost doubled in the last decades. Dyslipidemia is poorly managed by Egyptian doctors. According to the Egyptian DYSIS study (2013) , despite chronic statin treatment , two third of Egyptian patients had elevated LDL-C levels .
In Egypt mortality secondly to CHD is rapidly rising, According to WHO statistics the age standardized mortality rates from CHD are one of the highest worldwide.
Statin thereby is one of the greatest therapeutic advances in modern medicine, since they lower the risk of heart attack, stroke and death in high risk patients. The initiation and monitoring of statin therapy is an important chapter in Egyptian guidelines.
- Why Egyptian guidelines? Why not follow the international guidelines?
The majority of international guidelines were developed in Western or rich countries with different ethnic background, dietary habits, life style and health care system. Majority of Egyptians are not medically insured and pay out of their own pockets for drugs and medical services. Therefore the new Egyptian Guidelines have to make a compromise between what is ideal supported by clinical trials and what is feasible. Unfortunately there are limited data and few clinical trials addressing the question of dyslipidemia among Egyptians. Therefore many of the recommendations in Egyptian guidelines are based upon consensus and expert opinion, Furthermore the international guidelines are lengthy Some exceeding 300 pages, somewhat complicated, not familiar to Egyptian doctors and may be difficult to apply.
- How the new Egyptian guidelines will differ from other guidelines?
An important component in management of dyslipidemia is CV risk assessment and identifying high risk individuals who might need immediate and aggressive therapy. The international guidelines use risk scoring systems which are not familiar to the majority of Egyptian doctors and their validity was not tested in Egyptian patients.
The risk scoring in the Egyptian guidelines was based upon the number and intensity of CV risk factors. Patients were categorized into four groups:
- Low risk with no or just a mild risk factor
- Moderate risk with 2 -3 risk factors not including diabetes
- High risk patients with more than 3 CV risk factors, very high single risk factor, long standing diabetes or CKD.
- Very high risk patients with established atherosclerotic CV disease – coronary, cerebral, peripheral, carotid and aortic. Patients with acute coronary syndromes or acute stroke belong to this very high risk group.
The target LDL-C was a bit higher in the Egyptian guidelines. Though it is an established fact that the lower LDL-C the better and very low level (< 50mg / dl )are recommended in the very high risk patients ,this may not be feasible unless high dose of statins are prescribed or very expensive medications (PCSK9- inhibitors ) are administrated . This policy though it may look ideal, it cannot be followed in developing countries with low resources settings and for prolonged lifelong treatment.
- Who are the target audience?
Cardiologist and physicians in different specialties particularly endocrinology, diabetes and metabolism will find these guidelines useful in every day clinical practice.
- How guidelines were made?
a) The guidelines main author reviewed eleven national and international guidelines in addition to recent world literature. Important information was marked and collected as a reference.
b) A guidelines writing group was selected by the main author
c) Guidelines were classified into 7 chapters after an introduction , these chapters covered :
- Lipoprotein metabolism
- Assessment of global CV risk
- When to initiate and how to monitor statin therapy
- What is the role of other lipid lowering drugs
- Management of dyslipidemia in specific groups
- When and how to treat hypertriglyceridemia?
- Non pharmacological treatment.
d) Each of the writing group members was assigned one or more chapters.
e) Writing group members met on three occasions and a provisional draft was prepared and approved by all members
f) An advisory board was selected from experts in different specialties including general medicine, cardiology, endocrinology, and nephrology.
g) The final draft prepared by the writing group was send to the advisory board members for revision, comments and approval.
h) The writing group and advisory board met in joint meetings for final approval of guidelines and discussing future plans for guidelines dissemination and implementation.
- Guidelines dissemination and implementation
- After being approved by the advisory board guidelines are printed and sent to the heads of cardiac and medical departments in different universities, deans of medical schools and ministry health authorities.
- An educational program based upon the guidelines is prepared for physicians education to be organized in national meetings
- Guidelines will appear on the website of the EHS.
Antithrombotic Therapy
New Oral Anticoagulant and Antiplatelet Drugs
President Message
Part II
(January 2022)
M. Mohsen Ibrahim, MD
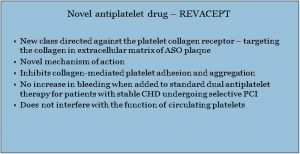
Antiplatelet Drugs
ROLE OF BLOOD PLATLETS
Form a platelet plug or thrombus to prevent blood loss when a blood vessel is injured. They are the first hemostatic mechanism.
Platelets normally circulate in blood as inactive tiny discs (2-3 microns in diameter) without nuclei and have smooth cell membrane which is very rich in platelet receptors.
When endothelium is injured or disrupted with exposure of the sub-endothelial matrix proteins and cells, adhesion proteins mainly collagen and von Willebrand factor adhere to platelets leading to platelets activation.
Platelet activation results in: (1) change in platelet shape from smooth discs to spiny spheres, (2) secretion of platelet contents such as serotonin, ADP, arachidonic acid, thrombin, fibrinogen, and adhesion proteins, (3) exposure and activation of GP IIb/IIIa receptors which are fibrinogen receptors. Fibrinogen forms cross bridges between activated platelets resulting in formation of platelet aggregates.
In the absence of cardiac arrhythmias and valvular heart disease, prevention of coronary thrombosis mainly relies on antiplatelet therapy.
Antiplatelet Drugs
– Aspirin
Inhibits cyclooxygenase enzyme (coxi), an enzyme responsible for the generation of thromboxane. Coxi converts arachidonic acid into the prostaglandin GZ, a precursor of prostaglandin PGH2.
PGH2 is either converted into prostacyclin-by-prostacyclin synthase present in endothelial cells or converted into TXA2 by thromboxane synthase in platelets.
Low dose aspirin inhibits platelet synthesis of thromboxane, while maintain endothelial synthesis of prostacyclin.
In addition to antiplatelet activity aspirin reduces markers of inflammation.
– P2Y12 Inhibitors: Thienopyridines:
Clopidogrel – Prasugrel – Ticagrelor
Block the binding of adenosine diphosphate (ADP) to a specific platelet receptor P2Y12.
Thienopyridines indirectly inhibit the activity of other platelet agonists such as arachidonic acid, collagen, thrombin, epinephrine, and serotonin. Also, they inhibit platelet aggregation induced by collagen and thrombin.
Clopidogrel and prasugrel are prodrugs, while ticagrelor is an active drug with additional active metabolites. Antiplatelet potency is greatest with prasugrel and less with clopidogrel and moderate with ticagrelor.
– Clopidogrel Vs. Ticagrelor
Ticagrelor is more effective, and for patients with ACS, it quickly inhibits platelet aggregation, while clopidogrel is less effective.
Clopidogrel is a prodrug, its activation can be influenced by genetic factors with some patients have clopidogrel resistance. Its onset of action is somewhat delayed and initial large loading dose is required.
In ACS treatment with ticagrelor as compared with clopidogrel significantly reduced the rate of death, myocardial infarction, and stroke without an increase in major bleeding.
Dual Antiplatelet Therapy (DAPT)
Combination of aspirin with oral antiplatelets (Clopidogrel, Ticagrelor).
Goals of DAPT are to prevent new ischemic events and prevent stent thrombosis.
DAPT indications:
1. Post-ACS event: patients have more thrombotic phenotype, 12 months DAPT is recommended regardless of stent placement.
2. Stable ischemic heart disease is less thrombotic phenotype and DAPT is considered if a stent is placed.
3. Severe diffuse atherosclerosis, high risk patients with peripheral artery disease and cardiovascular disease specially if combined with CAD.
Clopidogrel with aspirin are given to patients with TIA or minor stroke. Treated within 24 hours after onset of symptoms. The combination is superior to aspirin alone for reducing the risk of stroke in the first 90 days.
Duration of DAPT:
– Following ACS with stent or not: 12 months.
– Stent placed in non-ACS setting: 6 months.
The ESC/EASD guidelines highlighted the superiority of modern P2Y12 inhibitors and encouraged the use of these agents for DAPT in diabetes.
Long term therapy with aspirin and ticagrelor in diabetes patients with established CAD- for a median of 33 months-reduced major adverse cardiac events beyond 12 months of the coronary event.
More studies are required to understand the best strategy for long-term antithrombotic therapy in diabetes. The enhanced thrombotic environment in diabetes calls for alternative antithrombotic treatment strategies in primary and secondary vascular protection.
Triple Therapy
Aspirin + P2Y12 inhibitor + Oral anticoagulant
Rarely indicated beyond are month duration.
P2Y12 inhibitor (clopidogrel, ticagrelor) are preferred over aspirin: NOACs are preferred over warfarin.
Continue triple therapy for maximum one month post-hospital discharge.
When transition to dual therapy drop aspirin and continue P2Y12 inhibitor.
Choose NOAC rather than warfarin unless contraindicated or cost.
When Prescribing New Antiplatelet drugs consider the following factors:
1. Potency: Prasugrel most potent, followed by ticagrelor, then clopidogrel
In the ACS setting, we tend to prefer more potent agents like ticagrelor or prasugrel in the absence of contraindications
2. Bleeding risk: Increased bleeding risk is always the tradeoff of increased potency. We avoid prasugrel in patients age > 75, history of TIA/stroke, and hepatic dysfunction Also avoid ticagrelor in patients with history of ICH
3. Feasibility- Side effects: Ticagrelor inhibits adenosine reuptake, which can cause bradycardia and dyspnea, sometimes resulting in patient self-discontinuation.
4. Dosing frequency: Clopidogrel and prasugrel are once per day, while ticagrelor is twice per day
5. Price: Clopidogrel is the least expensive.
President Massage
Hypertension – Drug treatment Strategies in Daily practice
M. Mohsen Ibrahim, MD
This massage is derived from a lecture I gave in an international meeting held in Cairo this year. The information in the lecture was derived from world literature, recent guidelines and author’s personal experience while caring for hypertensive patients over more than fifty years.
The massage addresses the following six questions:
- When to initiate drug treatment for hypertension?
- Which drug is the first choice?
- How to monitor drug treatment?
- What to do about BP variability?
- How to manage poor BP control and resistant hypertension?
6. What is the role of new anti-hypertensive drugs?
The massage consist of 2 parts in part I will address the first two questions.
Part I
1. When to initiate drug treatment for hypertension?
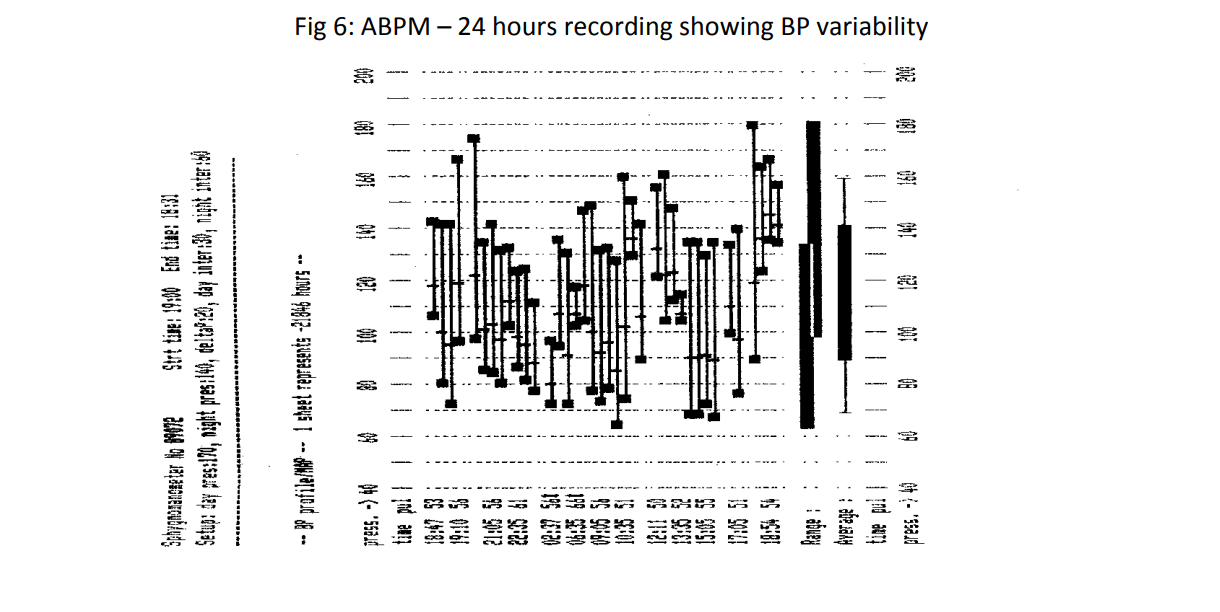
This is possibly the most important question. The decision to initiate drug treatment should not be taken lightly because once drug treatment for hypertension is started, it will continue indefinitely, since there is no cure from established essential hypertension. Before initiating treatment the physician should confirm the diagnosis of hypertension and assess the need and urgency for drug treatment. Accurate and repeated BP measurements are required before making the diagnosis in the office. Unless there is an urgency more than one office visit is required. Home BP measurements are sometimes necessary before making the diagnosis. However, 24 hours ambulatory BP measurements (ABPM) are possibly the best diagnostic method. We can reduce the number of patients starting treatment by 25 % if we use ABPM.
At initial evaluation it is necessary to assess the patient’s global CV risk and presence of target organ damage in order to determine the need and urgency for drug treatment.
The following table shows the definition and classification of hypertension based upon office readings according to recent guidelines
- Normal BP: <130/85 mmHg
- High normal BP: 130-139 and /or 85-89 mmHg
- Grade I HTN (mild): 140-159 and/or 90-99 mmHg
- Grade II HTN ( moderate): ≥160-179 and/or 100-109 mmHg
- Grade III HTN ( severe): ≥180 and / or ≥ 110 mmHg
- Isolated systolic HTN: ≥140 and ≤90 mmHg
The criteria for diagnosis of HTN very according to the method of measurement of BP. For the clinic (office) BP > 140/90 mmHg, for 24 hours ABPM > 130/80 mmHg, for home BP measurements > 135/85 mmHg and for automated office measurements > 135/85 mmHg. Home BP measurements are more reliable predictor of prognosis than clinic BP.
What is next after establishing the diagnosis of HTN?
Unless there is an urgency a trial of non-pharmacologic treatment in terms of lifestyle modification ( LSM) should be started and continued in parallel with drug therapy. Non- pharmacologic treatment includes weight reduction if obese, a healthy diet (DASH diet) rich in fruits, vegetables, fish, whole grain and cereals. Limiting salt intake to less than 5 gram sodium chloride / day is recommended, while avoiding sugary and high caloric drinks and foods rich in animal fat. Regular physical exercise e.g 30 minutes brisk walking/day while avoiding tobacco and alcohol are stressed.
Guidelines differ regarding the duration of the period of initial BP monitoring before initiating drug treatment. French recommended commencing pharmacologic treatment at stage 1- HTN regardless of other CV risk factors. However, the majority of guidelines recommended a trial period of LSM before drug therapy. The period varies from 3 months in the AHA/ACC guidelines and 6-12 months in ASH/ISH guidelines.
Immediate, initiation of drug therapy on first office or hospital visit according to Egyptian guidelines is indicated in hypertensive emergencies, when BP exceeds 210/120 mmHg on 3 consecutive measurements 2-3 minutes apart after excluding a panic attack or when BP is greater than 180/110 mmHg on 3 consecutive measurements in presence of target organ damage , symptomatic CV disease or chronic kidney disease(CKD).
2. Which drug is the first choice?
Anti-hypertensive drugs belong to five different pharmacologic groups besides new emerging drugs. The pharmacologic groups are thiazides and thiazide derivatives, RAS blockers, ARBs, sympatholytics and vasodilators.
These drugs address four different presser mechanisms responsible for BP elevation namely sympathetic over activity, RAS activation, increased blood volume and increased arterial stiffness. The choice of anthi-hypertensive drug group will depend upon patient’s age, CV risk factors, clinical CV disease and comorbidities such as diabetes mellitus (DM), CKD, obesity, heart failure, coronary artery disease (CAD), prostatitic hypertrophy, pregnancy, COPD, anxiety, migrain and tachycardia.
Diuretics are recommended in elderly patients, presence of heart failure (HF), CKD, renal failure and isolated systolic HTN.
Diuretics are the only drug class that targets a known cause of HTN, namely increased blood volume. Chlortholidone is superior to hydrochlorathiazide (HCTZ) in preventing CV events. Thiazides, or thiazide-like diuretics are effective down to an eGFR of 25-30 ml/min/ 1.73 m2. Below this eGFR level a long acting loop diuretic e.g (torsemide) should be used.
The side effects of diuretics include excess urination, hypokalemia, hyperuricemia and impaired glucose tolerance.
Calcium channel blockers (CCB) e. g. amlodipine are recommended in elderly patients and presence of CAD or peripheral arterial disease, pregnancy, excess BP variability and arrhythmias ( non-dihydropyridine CCBs). The side effects of CCBs include ankle swelling, headache and flushing. Recent CCBs like nicardipine have the advantage of less ankle edema and greater renal protection.
Beta-drenergic blockers (BABs) are indicated in presence of CAD, HF, arrhythmias, tremors, migrain, tachycardia, anxiety, hyperkinetic circulation and young age. Side effects of BABs are bradycardia, fatigue, impotence, exacerbation of bronchial asthma, cold extremities and worsening symptoms of peripheral vascular disease.
ACE inhibitors and ARBs are the drugs of choice in diabetic patients, HF and CKD. Side effects of ACE inhibition are cough, allergic reactions, hyperkalemia and rise in serum creatinine. ARBs have the advantages of less side effects (cough) compaired to ACE inhibitors. ARBs because of rare side effects enjoy the longest adherence to treatment.
RASBs Independent of their antihypertensive effect, have a cardioprotective effect in patients with high risk of CV disease.
ARBs adherence to treatment after 12 months is in 64% of patients compaired to 58% with ACE inhibitors, 50% with CCBs, 43% with BABs while thiazide diuretics have the lowest rate of 38% according to data from USA.
Less than half of all hypertensive patients will attain target BP with monotherapy, while 75% do not have optimal BP control. On the other hand 30% of patients will need 3 or more drugs in combination to attain target BP levels. The ability of any agent to achieve target BP (< 140/90 mmHg) when used alone does not exceed 20-30%.
When selecting first line therapy there are a number of compelling indications and choice of drug therapy will be individualized. The drugs of choice in hypertensive patients with angina are BABs ± CCBs, after MI or CABG are BABs ± (ACEIs or ARBs in HF diuretics + BABs+ RASBs. In cerebrovascular disease or PAD, RASBs+ CCBs, in pregnancy methyl dope ( aldomet) and CCBs, in prostatic hypertrophy alpha adrenergic blockers (doxazosin). BABs are recommended in presence of migrain, tremors and situational anxiety.
President Massage
Hypertension – Drug treatment Strategies in Daily practice
Part II
3. How to monitor drug treatment?
Clinical evaluation and BP check are required every 2-4 month, while laboratory
monitoring for blood chemistry and ECG may be needed once / year unless there are
specific indications.
Fig 4: Initiation and Monitoring of Drug Therapy
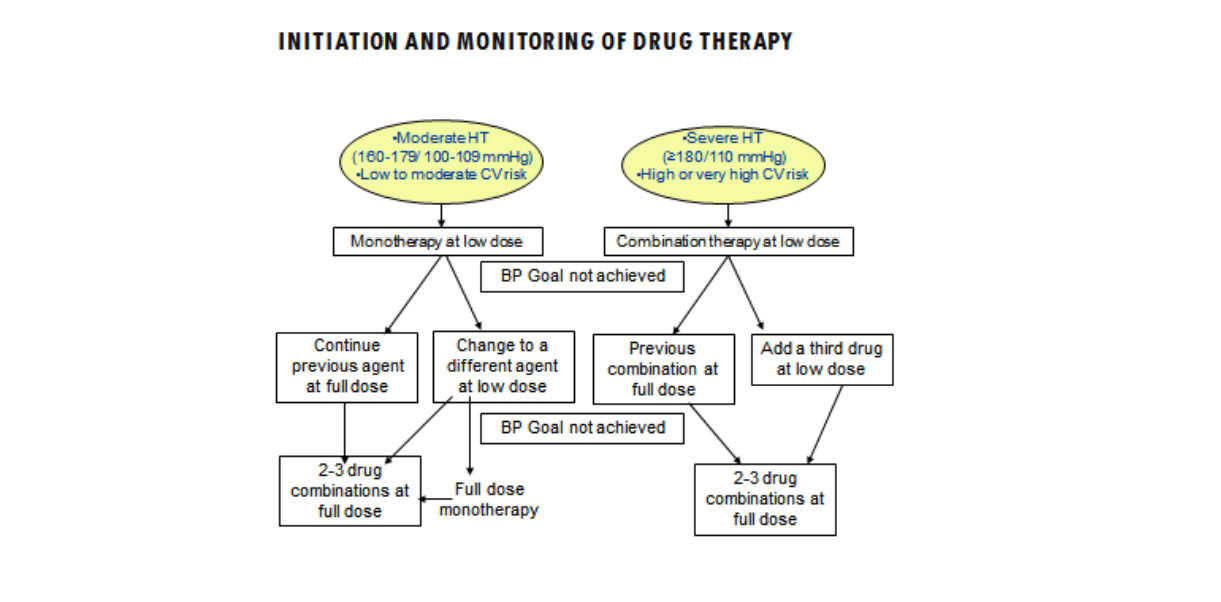
Hypertension – drug treatment strategies in daily practice. M. Mohsen Ibrahim
Antihypertensive drugs may require a period of up to two months to achieve maximal hypotensive effect. On the other hand a significant reduction in BP can be achieved after two weeks of therapy with many drugs, particularly combination therapy. It is not
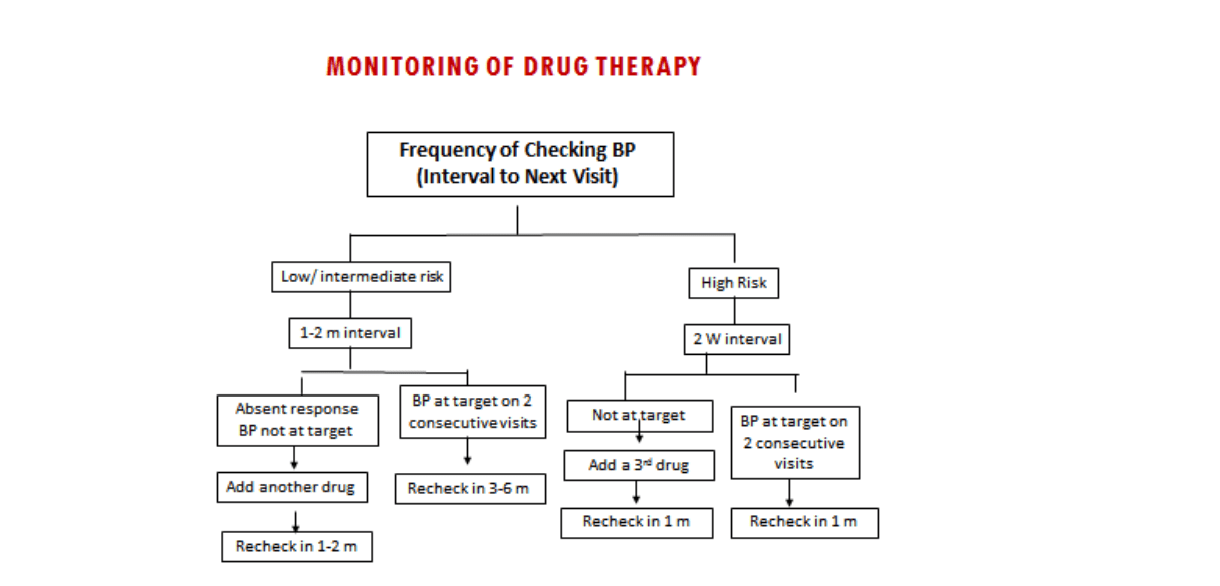
recommended to change drugs at short intervals. It is advisable to recheck BP at one to two monthly interval until it remains at target level for two consecutive visits, then recheck at 3-6 months depending upon the CV risk profile. Frequency of checking BP
(interval to next visit) in low to intermediate risk patients is at 1-2 months intervals, while in high risk patients at two weeks intervals. Recent guidelines define BP control as < 130/80 mmHg in the office and <125/75 mmHg as determined by 24 hours ABPM
Fig 5: Monitoring of drug therapy frequency of checking BP
To improve patients compliance with antihypertensive drugs, patients education is recommended stressing the fact that HTN is silent, dangerous if not treated , requires life-long treatment and monitoring. Physician should prescribe affordable drugs while
drug administration is preferably once daily with minimal number of tablets, better a single pill combination.
4. What to do about BP variability?
Levels of BP are liable to fluctuation and can change from minute to minute and from day to day . These fluctuations in BP can generate anxiety and confusion regarding diagnosis and treatment.
Short term BP variability may be instantaneous within seconds as occurs during sleep, pain, posture , emotions, talking, distended urinary bladder or within minutes after smoking, meals, hypoglycemia or within hours following medication or circadian-diurnal changes. Long term or office visit to visit variability can be spontaneous , due to drugs or rarely pheochromocytoma.
Guidelines regard variability of BP as noise that has to be removed from the diagnostic process and that HTN should not be diagnosed on the basis of episodic rises in BP unless mean BP is raised ( ESH 2007 guidelines). Guidelines differ regarding the management of BP variability. Some stress the need to do 24 hours ABPM or home measurements (ESH 2007), others stress the need to confirm BP elevation in 2-5 subsequent visits ( JNC, BHS and Canadian guidelines).
The treatment implication of reducing visit to visit BP variability are uncertain and there is no direct evidence that a reduction of visit to visit variability (VVV) is beneficial. However, CCBs and diuretics tend to decrease VVV, whereas BABs and RASB seem to do the opposite.
5. How to manage poor BP control and resistant hypertension?
Failure to achieve optimal BP control is responsible for 60% of cerebrovascular accidents, 50% of coronary events, for 7.1 million death/year and 64.3 million serious disabilities/ year. It is predicted that over the next 10 years health costs of non-optimal BP are likely to reach over 908 billion dollar if BP remains at current levels. Optimal BP control varied in hypertension surveys from 23% in USA, 24% in France, 16% in Canada, 8% in Egypt and 5% in China.
The causes of poor BP control may be drug, lifestyle or physician related. Drug related causes include limited access to treatment, poor adherence or inadequate,dosage. Lifestyle causes are unhealthy diet, excess salt intake, obesity, sedentary
lifestyle and continuous emotional stress. Lack of adherence to treatment guidelines, inadequate follow-up, therapeutic inertia and lack of adequate time with the patient are physician and health system related causes.
In an Egyptian survey of 1534 hypertensive patients up to 79% of patients quite treatments within the first year. Only 10-15% of originally treated patients were still adherent to treatment after five or more years.
Resistant Hypertension
Definition (AHA 2018) of resistant HTN:
Above goal BP despite 3 or more BP medications commonly including a long acting
CCB, RAS blocker and a diuretic at maximally tolerated doses and appropriate
dosing frequency, excluding white coat HTN with ABPM or home monitoring and
medication non-adherence. This definition excludes causes of false resistance.
Management of resistant HTN
First exclude pseudo-rsistance by accurate BP measurement, ensuring adherence to lifestyle modification and antihypertensive therapy. ABPM (24 hours) and if unavailable use home BP in order to exclude white-coat HTN. Also history of intake of pressor drugs and obstructive sleep apnea should be excluded, then increase the dose of diuretics since blood volume expnasion is an important cause of resistant HTN. Long acting loop diuretic is added and if fail add spironolactone.
Assess for secondary HTN if still BP is not controlled after the previous measures. Causes include primary aldosteronisne , renal parenchymal disease, renal artery stenosis, pheochromocytomar, paraganglioma, Cushing syndrome, coarctation of
the aorta and other endocrcine causes.
What to do if there is inadequate BP response?
1. Exclude :
a. Pseudo resistance and white coat effect
b. Intake of pressor drugs
c. Obstructive sleep apnea
2. Stress lifestyle modification:
a. Limiting salt intake
b. Treat obesity
c. Stress management
3. Pharmacologic treatment:
a. Blood volume control: aggressive diuresis-use loop diuretics
b. Aldactone/ spironolactone
c. BABs if heart rate is >70 b/m
d. α-blockers and vasodilators if heart rate < 70 b/m
4. If fail screen for secondary hypertension
6. What is the role of new anti-hypertensive drugs?
Many of the following drugs are not yet established standard treatment for HTN, but
may be part of the future drug therapy of HTN. The list of new antihypertensive drugs
include:
1. New calcium channel blockers
2. Endothelin antagonists
3. Combined ARB with a Neprilysin inhibitor
4. Aldosterone synthase inhibitors
5. Natriuretic peptide receptor agonists
6. Imidazole’s: centrally acting drugs with less side effects
7. Neutral endopeptidase inhibitors : inhibit metabolism of atrial natriuretic peptide .
8. Mineralocorticoid receptor antagonists.
1. New calcium: channel blockers:
Third generation CCB have less incidence of peripheral edema in hypertensive patients which improves drug persistence in treated patiens. Examples of new CCBs are lercanidipine, lacidipine and manidipine
2. Endothelin antagonists:
Because of their side effects ( headaches and fluid retention) they are only used in resistant hypertension or hypertension of renal disease.
3. Combined ARB with a Neprilysin inhibitor:
Neprilysin is the enzyme when breaks down natriuretic peptides. Sacubitril is a neprilysin inhibitor which enhances the vasodilation of these peptides. The combination with an ARB ( valsartan) is commercially available ( Entresto) which is used in treatment of heart failure and resistant hypertension.
4. Aldosterone synthase inhibitors:
LCI699 is the first orally active aldosterone synthase inhibitor for human use. It decreases plasma and urine aldosterone concentration. New compounds as potent and more selective than LC I 699 are currently being tested as treatment for mineralocorticoid dependent CV and renal disease.
5. Natriuretic peptide receptor agonists:
Increased natriuresis and diuresis, elevate plasma cyclic guanosine monophosphate and reduce systemic BP. PL- 3994 given subcutaneous with prolonged half life administered as an adjunct to standard therapy in patients with resistant HTN. It has reduced affinity for the natriuretic peptide clearance receptor and increased resistance to neprilysin.
6. Mineralocorticoid receptor antagonists:
Spironolactone has significant progesterone and antiandrogenic activity. Eplerenone is more selective MRA but is less potent. Finerenone, a non-steroidal MRA is more selective than spironolactone and more potent than eplerenone
Summary and Conclusion
Drug treatment of HTN has changed the outcome of hypertensive patients and is one of the most successful therapeutic achievements.
However, drug treatment does not provide cure for HTN, therefore it has to be continued indefinitely to maintain BP control. The first and possibly most critical question is when to start drug treatment. The answer depends upon the accurate diagnosis of HTN and the detection of other CV risk factors. The threshed for diagnosis of HTN depends upon the method of BP measurement and recommendation of guidelines. Office measurements have obvious limitations and recent guidelines do not depend upon office readings to establish the diagnosis and initiate therapy. ABPM and automated office measurements provide more accurate and reliable methods to diagnosis HTN. After deciding the need for drug treatment the next question is which drug to choose as initial therapy. This will depend upon patient’s age, drug cost, presence of target organ damage and co-morbid conditions. Drug combination therapy is recommended in the majority of patients mainly ACEIs, ARBs combined with CCBs and or thiazide diuretics. These agents are specially recommended in patients with CKD, DM, HF. In presence of CAD, BBs are the first choice. In elderly atients and in presence of isolated systolic HTN,CCBs and diuretics are drugs of first choice. BBs are recommended in presence of CAD, HF, tachycardia, anxiety, migraine and arrhythmias. Drug therapy requires careful monitoring. BP should be checked at 2-4 weekly intervals after initiation of treatment, then at 2-6 monthly intervals depending upon BP level and CV risk profile. BP variability is a
common problem and diagnosis of HTN should not be made unless the BP is persistently elevated. Failure to achieve optimal BP control is another common problem: Interruption and/or inadequate drug therapy is the main cause. Patients education is mandatory, stressing the silent nature of HTN and the need to continue drug therapy indefinitely. Doctors should be aware of the recent guidelines and the importance of single pill combination and regular BP monitoring. Management of true resistant HTN (after exclusion of white coat HTN), depends upon accurate diagnosis, lifestyle modification ( low salt) weight reduction, avoiding presser medications and treatment of obstructive sleep apnea. Increasing the dose of diuretics and use of spironolactone are recommended in truely resistant cases. Finally there is a rapidly growing list of new ntihypertensive drugs which are undergoing clinical trials and can be used as a last resort in truely resistant hypertensive patients.
President Massage
Towards an Ideal Antihypertensive Drug
M. Mohsen Ibrahim, MD
Prof. of Cardiology – Cairo University President of the Egyptian Hypertension Society
Once diagnosed established essential hypertension (HTN) mandates a lifelong drug therapy since here is no permanent cure from established essential HTN. Pharmacologic therapy in addition to its cost carries the risks of side effects, failure to target the presser mechanisms, prevent progression of target organ damage and address associated CV risk factors commonly present in hypertensive patients. Therefore, an ideal antihypertensive drug should be affordable, orally effective in lowering BP, capable of preventing and regressing target organ damage, free from side effects and can address other associated CV risk factors. The choice of one drug over another should ideally be supported by good clinical evidence. The therapeutic effect of the drug is expected to be maintained throughout the 24 hours dosing interval. A longer half life is a therapeutic advantage which can cover the early manning risk of BP when acute hypertensive life-threatening complications occur.
Inflammation might contribute to the development of HTN and its complication. Antihypertensive drugs with anti-inflammatory potential provide a definite advantage. Lowering of markers of inflammation was reported with some antihypertensive medications. Inflammation plays a central role in development of atherosclerotic lesions and CV events. Drugs that lower markers of inflammation in hypertensive patients will help in prevention and regression of atherosclerotic lesions.
Endothelial dysfunction is an early event in vascular pathophysiology and is implicated in HTN and atherosclerosis. An ideal antihypertensive will have beneficial effects on endothelial function.
Reduction in arterial stiffness which is commons in elderly hypertensive patients is a pre-requisite for an ideal antihypertensive drug.
Prevention and regression of hypertensive complications namely LV hypertrophy, atherosclerosis and renal dysfunction are mandatory for an ideal antihypertensive drug. LV hypertrophy in hypertensive patients significantly increases the risks of coronary heart disease, stroke arrhythmias and heart failure. Reduction in LV mass and left atrial size can prevent or delay the recurrence of atrial fibrillation and HF. Prevention and regression of LV hypertrophy are important targets of therapy.
Insulin resistance and diabetes are common among hypertensive patients. An ideal drug will improve insulin resistance and help prevent diabetes. On the other hand lowering of glomerular pressure will prevent progression of diabetic nephropathy and prevent the decrease in glomerular filtration rate (GFR) in patients with micro or macro albuminuria.
It is expected that an ideal agent will not only effectively lower BP but can improve glucose and lipid metabolism and regress inflammatory markers and target organ damage.
President Massage
EHS Activities for the year 2023
The Society will continue activities started in 2022, namely the national hypertension prevention program (NHPP) and the recently formed advisory board activities, in addition to the annual and summer meetings, website and hypertension club activities.
The NHPP which is a nationwide prevention program aims to decrease the prevalence of hypertension (HT) among Egyptians through increasing public awareness regarding healthy lifestyle, limiting salt intake, control of obesity and regular physical exercise. These approaches proved effective in prevention of HT in a number of countries. The nationwide Egyptian program includes visits by program experts to different governorates, during one day meeting lectures are given to the public and local doctors explaining the different approaches for hypertension prevention. During the visits BP was checked, data were collected about lifestyle, drug intake and health condition from public attending the meetings. Doctors and pharmacists were instructed how to measure BP accurately. The information collected from the public regarding HT knowledge, treatment and attitude may serve in planning future education programs and an epidemiologic research material.
In 2022 an advisory board from active Egyptian physicians was formed to share in the society activities. A number of meeting for the advisory board are planned in the year 2023.
It is our aim through the HT prevention program to decrease its burden in the community and limit its complication. We need to approach food industry, government authorities and legislative bodies to develop regulations regarding limiting salt intake and provide low salt healthy foods at restaurants and grocery stores.
In the year 2023 the society is planning to develop a number of publications for physician education. A writing group chaired by the society president will share in
writing at least three publications. The suggested topics are: HT in the elderly, antihypertensive drugs and curable forms of HT.
The annual scientific meetings of the society will provide in addition to their physician education massage an opportunity to update Egyptian physicians regarding recent advances in the field of HT, including new mechanisms, diagnostic methods and treatment. Now we realize that HT is not a homogenous disorder and strategies to improve HT control may involve specific therapies for individual patients. HT related mechanisms differ among subgroups of patients, and BP responses to different classes of antihypertensive drugs vary among individual patients. The concept of physiologic profiling to guide the selection of specific classes of antihypertensive agents for individual patients has the potential to increase the effectiveness of the drug.
The EHS welcomes the contribution of all physicians and scientists interested in HT to its educational and scientific activities; the society website under the supervision of Dr. Ghada Sayed is the window of the society on national and international HT worlds and is an excellent opportunity for physician education and public awareness. Let us look for a productive and successful 2023.
President Massage Hypertension in the Elderly
M. Mohsen Ibrahim, MD
Prof. of Cardiology – Cairo University President of the Egyptian Hypertension Society
Worldwide life expectancy has increased significantly particularly in industrialized countries. At the beginning of the 20th century life expectancy was between 30 and 45 years. At the end of the century, life expectancy 67 years. The over 80’s are the fastest growing group on the planet. In 20 years, the aged population is estimated to exceed almost 20% of the whole population. Hypertension is the leading cause of cardiovascular (CV) morbidity and mortality in adults over the age of 65. The estimated prevalence of HT in the elderly is around 60- 70%. This message will address the following questions:
- What is the definition of elderly?
- What are the mechanisms of hypertension in the elderly?
- What are the clinical and hemodynamic characteristics?
- What are the challenges in management?
- Whom to treat, to what target and with which drug class?
- Definition of the elderly: Old age is officially defined by 60 years according to the united nations. Sometimes 65 years is used as the cutoff point. While the very elderly are older than 80-85 years.
- Mechanisms of HTN in the elderly: 85% of men and women with normal BP at age 55 years will develop HTN after 20-25 years of follow up. There are at least four mechanisms responsible for the higher prevalence of HTN in the elderly namely increased arterial stiffness, endothelial dysfunction, a proinflammatory state associated with aging and sodium retention. Arterial stiffness develops as a consequence of wall hypertrophy, calcification and atheromatous lesions and changes in exliocellular matrix which include an increases in collagen and fibronectin, fragmentation and disorganization of the elastin network.
Endothelial dysfunction resulting in reduction in endothelial- dependent vasodilation secondly to diminished capability to generate NO by the endothelium and decrease of vasodilation receptors. Vascular oxidative stress and inflammation significantly increase with age which result in reduction of NO bioavailability and decreased vasodilator capacity. Sodium retention is more likely in the elderly secondary to progressive deterioration of renal function and reduction in the nephron population.
Clinical and hemodynamic characteristics
These can be both age related and hypertension related changes. Age related changes include reduced cardiac B-receptor mediated responsiveness resulting in tendency for slowed heart rate and decreased heart rate response to exercise. Large artery stiffness leads to impaired activation of the baroreflex . In the
elderly there is a tendency to left ventricular hypertrophy independent of HTN. Also there is delayed excretion of salt/ volume leading to impaired ability to maintain normal fluid volume. Co-morbid conditions are more common with advancing age and include diabetes mellitus depression, fraility ; foot and leg edema, and osteoarthritis .
Hypertension related changes include the greater prevalence of atherosclerotic arterial disease, ischemic cardiac and renal disease, tendency to arrhythmias, abdominal aortic aneurysm, impaired LV function, diabetes and sleep apnea.
Challenges in management
There is a number of conditions that influence the outcome of hypertensive patients and can change the therapeutic strategies. These challenges are the presence of multimorbidety which means the presence of two or more long term conditions in additions to HTN e.g. diabetes mellitus, CAD, dyslipidemia, heart failure, CKD, AF, obesity, OSA, gout and depression. At least two thirds of hypertensive patients have another co-morbid condition. Polypharmacy common in hypertensive patients is associated with poor health outcomes secondary to falls, electrolyte disturbances, hospitalization, heart failure and premature mortality. Fraility which is reduced physiological reserve leading to incresed vulnerability to physical stressors is one
manifestation of aging. Tendency to orthostatic hypotension and falls, which are more common in the elderly is another challenge in management. Cognitive impairment is an additional problem in the elderly. The prevalence of dementia in the over 65 population is estimated at 6.5%.
Treatment
A target BP of < 150/ 90 mmHg is recommended to reduce CV morbidity and mortality in the elderly. The recommended BP goal in patients with history of stroke, diabetes or CKD is less than 140/80 mmHg.
Individualized decisions are recommended regarding initiation and choice of pharmacologic therapy after trial of dietary approaches. Limiting salt intake and a healthy lifestyle is important. Unless there are specific indications, thiazide diuretics are the first choice.
The choice of therapy is guided by patients preference and comorbidities. To start low, go slow approach to medication prescribing is an important approach. The benefits of antihypertensive therapy in reducing hypertensive complications is largely driven by the lowering of BP rather than the choice of drug. On the other hand CCBs and ACEIs, may offer some protection against cognitive decline in older hypertensive patients.
Before starting treatment BP should be measured first supine followed by upright position to assess orthostatic reaction.
In short we are expecting to see an increasing member of elderly hypertensive patients in the coming years.
These patients are in need of lifelong treatment. Lifestyle modification and thiazide diuretics are recommended as initial therapy unless there are compelling indications for specific pharmacologic agents.
President Massage Hypertension in the Elderly
M. Mohsen Ibrahim, MD
Prof. of Cardiology – Cairo University President of the Egyptian Hypertension Society
Worldwide life expectancy has increased significantly particularly in industrialized countries. At the beginning of the 20th century life expectancy was between 30 and 45 years. At the end of the century, life expectancy 67 years. The over 80’s are the fastest growing group on the planet. In 20 years, the aged population is estimated to exceed almost 20% of the whole population. Hypertension is the leading cause of cardiovascular (CV) morbidity and mortality in adults over the age of 65. The estimated prevalence of HT in the elderly is around 60- 70%. This message will address the following questions:
- What is the definition of elderly?
- What are the mechanisms of hypertension in the elderly?
- What are the clinical and hemodynamic characteristics?
- What are the challenges in management?
- Whom to treat, to what target and with which drug class?
- Definition of the elderly: Old age is officially defined by 60 years according to the united nations. Sometimes 65 years is used as the cutoff point. While the very elderly are older than 80-85 years.
- Mechanisms of HTN in the elderly: 85% of men and women with normal BP at age 55 years will develop HTN after 20-25 years of follow up. There are at least four mechanisms responsible for the higher prevalence of HTN in the elderly namely increased arterial stiffness, endothelial dysfunction, a proinflammatory state associated with aging and sodium retention. Arterial stiffness develops as a consequence of wall hypertrophy, calcification and atheromatous lesions and changes in exliocellular matrix which include an increases in collagen and fibronectin, fragmentation and disorganization of the elastin network.
Endothelial dysfunction resulting in reduction in endothelial- dependent vasodilation secondly to diminished capability to generate NO by the endothelium and decrease of vasodilation receptors. Vascular oxidative stress and inflammation significantly increase with age which result in reduction of NO bioavailability and decreased vasodilator capacity. Sodium retention is more likely in the elderly secondary to progressive deterioration of renal function and reduction in the nephron population.
Clinical and hemodynamic characteristics
These can be both age related and hypertension related changes. Age related changes include reduced cardiac B-receptor mediated responsiveness resulting in tendency for slowed heart rate and decreased heart rate response to exercise. Large artery stiffness leads to impaired activation of the baroreflex . In the
elderly there is a tendency to left ventricular hypertrophy independent of HTN. Also there is delayed excretion of salt/ volume leading to impaired ability to maintain normal fluid volume. Co-morbid conditions are more common with advancing age and include diabetes mellitus depression, fraility ; foot and leg edema, and osteoarthritis .
Hypertension related changes include the greater prevalence of atherosclerotic arterial disease, ischemic cardiac and renal disease, tendency to arrhythmias, abdominal aortic aneurysm, impaired LV function, diabetes and sleep apnea.
Challenges in management
There is a number of conditions that influence the outcome of hypertensive patients and can change the therapeutic strategies. These challenges are the presence of multimorbidety which means the presence of two or more long term conditions in additions to HTN e.g. diabetes mellitus, CAD, dyslipidemia, heart failure, CKD, AF, obesity, OSA, gout and depression. At least two thirds of hypertensive patients have another co-morbid condition. Polypharmacy common in hypertensive patients is associated with poor health outcomes secondary to falls, electrolyte disturbances, hospitalization, heart failure and premature mortality. Fraility which is reduced physiological reserve leading to incresed vulnerability to physical stressors is one
manifestation of aging. Tendency to orthostatic hypotension and falls, which are more common in the elderly is another challenge in management. Cognitive impairment is an additional problem in the elderly. The prevalence of dementia in the over 65 population is estimated at 6.5%.
Treatment
A target BP of < 150/ 90 mmHg is recommended to reduce CV morbidity and mortality in the elderly. The recommended BP goal in patients with history of stroke, diabetes or CKD is less than 140/80 mmHg.
Individualized decisions are recommended regarding initiation and choice of pharmacologic therapy after trial of dietary approaches. Limiting salt intake and a healthy lifestyle is important. Unless there are specific indications, thiazide diuretics are the first choice.
The choice of therapy is guided by patients preference and comorbidities. To start low, go slow approach to medication prescribing is an important approach. The benefits of antihypertensive therapy in reducing hypertensive complications is largely driven by the lowering of BP rather than the choice of drug. On the other hand CCBs and ACEIs, may offer some protection against cognitive decline in older hypertensive patients.
Before starting treatment BP should be measured first supine followed by upright position to assess orthostatic reaction.
In short we are expecting to see an increasing member of elderly hypertensive patients in the coming years.
These patients are in need of lifelong treatment. Lifestyle modification and thiazide diuretics are recommended as initial therapy unless there are compelling indications for specific pharmacologic agents.
President Massage Reversible Causes of HTN
- Mohsen Ibrahim, MD
Prof. of Cardiology – Cairo University President of the Egyptian Hypertension Society
June 2023
The search for a reversible or curable HTN is essential when discovering high BP in an individual. HTN once diagnosed will necessitate lifelong therapy and follow up, since there is no cure from established essential HTN. However, in some individuals when discovering high BP for the first time, the presence of reversible or curable cause should be considered. Severe anxiety, panic attacks and intake of presser drugs should be first excluded. Excess sympatho-adrenal stimulation is responsible for high BP in these individuals. Sudden appearance of HTN with severe headache is present in drug induced adrenergic HTN. Examples include overdose of amphetamines, appetite suppressants, phenyl ethanolamine, monoamine oxidase inhibitors with intake of tyramine rich foods. Sudden clonidine with drawal can lead to severe HTN due to activation of peripheral sympathetic tone. Treatment of this condition is restarting clonidine and IV phentolamine or labetalol. HTN can develop after intake of 9- Alpha fluro-cortisone and drugs causing salt and water retention such as corticosteroids and non- steroidal anti-inflammatory drugs (NSAIDs). Some nasal drops, drug for asthma, rheumatic disorders, acute pain, depression, apatite suppressants and oral contraceptives can induce HTN. Obstructive sleep apnea characterized by periods of interrupted breathing during sleep is a common cause of HTN in obese subjects. On the other hand, episodes of elevated BP in 10% of the day can be present in normal subjects probably related to anxiety, panic disorders or white coat HTN.
When drug intake is excluded as a possible cause of HTN, search should be made for other reversible causes. HTN due to narrowing of renal arteries is possibly the most common form of reversible HTN. The mechanisms include salt and water retention and excess renin production. Diagnosis of renal artery stenosis is suspected when auscultating renal area and discovery of abdominal bruits.
Laboratory and radiologic evaluation is needed which include measurements of plasma renin activity after oral captopril, rapid sequence IVP, Doppler flow measurement of renal arterial flow, digital subtraction renal angiography and MRI of renal arteries. Radio isotopic renography (renal scan) is possibly the best for non-invasive detection of renal artery stenosis. Rare causes of reversible renal HTN include renal artery stenosis secondary to compression of renal artery by tumor, dissection of renal arteries, neurofibromatosis, Takayasu-type granulomatous arteritis, renin secreting tumour and obstructive renal disease.
Adrenocortical HTN secondary to mineralo-corticoid excess though rare but potentially curable. It should be suspected in the presence of hypokalemia, reduced plasma renin activity, increased 24- hours urinary aldosterone and increased plasma aldosterone not reduced by high salt intake.
Pharmacologic blockade of aldosterone by high doses of spironolactone for 4-6 weeks, if BP falls to normal is an indication for surgery which will cure HTN.
Conditions which mimic primary aldosteronsm through the combination of HTN, hypokalemia and suppressed plasma renin include inherited disorders of steroid synthesis such as gluco-corticoid remediable aldosteronism, 11 OH hydroxylase deficiencies, leading to impaired cortisol synthesis resulting in increased ACTH secretion by the pituitary. Replacement with dexamethasone will suppress ACTH secretion to normal.
Pseudo aldosteronism follow prolonged ingestion of licorice which can lead to HTN and hypokalemia. Adrenal medullary tumors-Pheochromocytoma is a potentially curable form of HTN when diagnosed and surgically removed.
Cushing’s syndrome secondary to glucocorticoid excess is associated with HTN in 80 % of patients. Adrenal adenoma, carcinoma or pituitary adenoma, ACTH producing non-pituitary neoplasms are potentially curable forms of HTN after surgical removal of the tumor.Diagnosis is suspected by the presence of Cushingoid features namely moon facies, plethora, abdominal obesity and purple striae. Coarctation of the aorta is a potentially curable form of HTN and can be easily suspected on clinical grounds by discovery of weak and delayed femoral arterial pulsation, systolic murmurs and rib notching on chest X. ray.
Collagen vascular diseases such as scleroderma, polyarteritis nodosa, systemic lupus erythematosus, oral contiaceptive intake and toxemia of pregnancy are other potentially reversible causes of HTN.
Conclusion: the list of reversible causes of HTN is long and the careful clinician should always suspect the possibility of an underlying potentially curable cause before submitting his patient to a life long drug therapy. Exclusion of anxiety, panic, pressor drug intake should be considered before detailed radiologic and laboratory investigations.
President Massage
EHS Activities
By: M. Mohsen Ibrahim, MD
In the year 2022/2023 the EHS began two national activities namely: (1) National Hypertension Prevention program and (2) Hypertensive patient’s field survey
. The prevention program main objective is to decrease the incidence of HTN and the number of hypertensive patients in our country. Egypt has a high prevalence rate of HTN where more than one quarter of the population suffer from high BP. With advancing age more than half of Egyptians over the age of 60 years are hypertensive, according to the data of the Egyptian national hypertension project survey done in the early nineties. Obesity and high dietary salt intake, two risk factors for high BP are common among Egyptians. HTN is responsible for the large number of strokes, heart attacks, heart failure and renal failure among Egyptians.
The drug treatment of HTN and BP monitoring of the hypertensive patients are lifelong, which entail psychological and financial burden. In a number of countries such as UK, Japan, and Finland HTN prevention programs proved effective in decreasing the burden of HTN in the community. The Egyptian national hypertension program addresses the public, medical community, food industry and health authorities. The objectives are to increase public awareness of the risks of Hypertension and the different approachs for its prevention, based upon a healthy lifestyle, treating obesity and limiting salt intake. Dietary salt plays critical role in the development of HTN specielly in the vulnerable groups namely individuals with family history, renal disease and the elderly.
Limiting dietary salt intake proved effective in the prevention of HTN. In Western countries the main sources of salt in diet come from processed and canned foods, and foods served in restaurants. In other countries salt added during cooking and preparation of meals and at table is the main source of salt.
Public education and increasing public awareness are essential components in HTN prevention, stressing the risk of high salt intake and that diet with limited salt less than five grams /day can help prevent HTN. Public should identify food items rich in salt namely pickles, ketchup, canned foods, soup, vegetables and meat. Public awareness can be achieved through the media, press, TV, advertising in metro stations, shopping malls and through interactive meetings in doctor’s office,outpatient clinics, social and health clubs.
A healthy lifestyle is an important component in HTN prevention, this includes a diet rich in fruits and green vegetables, beans, nuts and low in saturated fat, sugar and salt.
Prevention and control of obesity through a low coloric diet and regular physical exercise is possibly the most effective non-pharmacologic method for the prevention of HTN and reduction of BP. Promotion of low salt and low coloric healthy food served in restaurants ,in grossery and food stores is recommended.
Encouraging regular physical exercise e. g. brisk walking 20-30 minutes /day is an important component in the healthy lifestyle and for prevention of obesity and Hypertension. Avoiding cigarettes smoking and excess alcohol are also mandatory.
Government authorities should develop laws and implement regulations directed to food industry and food serving places. All food items in restaurants, food stores and supermarkets should have a label indicating salt content of the food item. “We serve a healthy food” can appear on front door of restaurant and grocery store which will be a good incentive. Food menu will indicate the healthy food items which are low in salt and saturated fat.
The Egyptian HTN prevention program which includes public awareness and physician education started this year under the supervision of professor Dr. Wafaa El-Aroussy in Fayuom. The activity included besides regular lectures to doctors and public, BP checking stations and blood testing for sugar and lipid profile. The activity was repeated in Port Said and Kafr El-Sheikh.
Still missing is the approach to government and legislation authorities and contact with food industry to develop necessary regulation that help in the suress of the program.
The second important new EHS activity is a nationwide HTN field survey. The aim of this field survey is to collect data about the Egyptian Hypertensive patients regarding thair CV risk profiles, associated disease, hypertensive complications, type and compliance with antihypertensive medications, reasons for interruption of treatment, patients knowledge and attitude regarding HTN and his lifestyle. The data might help developing new recommendations and guidelines for the management of HTN in Egypt.
PRESIDENT‘S MESSAGE
Problem of Hypertension Diagnosis
JAN 2024
Diagnosis of hypertension depends upon accurate BP measurement and repeated BP readings. An accurate measurement will depend upon the equipment, technique, and approach whether office, home or ambulatory BP monitoring (ABPM). Repeated readings are taken through multiple office visits, repeated home measurements or 24 hours ABPM.
Accurate measurement requires a well calibrated machine and a trained observer familiar with the details of the technique and precautions taken when checking BP. Many doctors have no formal education on how to measure BP accurately. Ignorance regarding cuff selection and application, incorrect cuff positioning and rapid cuff deflation rate, inadequate rest period, digit bias and lack of repeated measurements will provide inaccurate readings. Faulty equipment- sphygmomanometer (mercury and aneroid) will give wrong numbers. In UK 44% of the aneroid sphygmomanometer used in hospital setting and 61% of them used in private medical practices were found inaccurate. Lack of calibration and maintenance of the aneroid sphygmomanometer makes them highly doubtful for routine use in medical practice, unless maintenance and calibration is implemented.
Blood pressure variability is an important limitation of casual BP office readings. The great diurnal variability inherent in BP behaviour, makes office measurement of limited diagnostic value. There is a need for repeated BP measurements before diagnosing hypertension. A single BP measurement would over-diagnose hypertension in 20- 30% of cases. Many people with current diagnosis of hypertension might not in fact have hypertension. Routine BP values obtained in the office are generally higher than high quality research readings. Blood pressure readings by primary care physicians tend to be higher than what it would be if measurements guidelines were strictly adhered to.
ABPM and home BP have a strong prediction power than conventional office BP for CV events. On the other hand, there is a gap between office and ABPM control. BP control is underestimated at the office (52% vs. 24%). We over-treat hypertension and that we could reduce the numbers starting antihypertensive treatment by 25% if we used ABPM instead of clinic BP to diagnose hypertension.
There is uncertainty around the current BP cut-off point (140/90 mmHg) consisting of huge number of people being misdiagnosed of having and not having hypertension. Over-diagnosis exposes people unnecessarily to considerable risk of adverse drug reactions.
The choice of a target BP < 140/90 mmHg regardless of underlying cardiovascular risk, intensity of treatment and underlying disease severity may not be a correct policy. Over-treatment and diastolic hypotension have been shown to be associated with worse cardiovascular outcomes.
The cut point for normal BP in the “real world” should be < 150/95 mmHg and not the value < 140/90 mmHg derived from research studies. Patients at low absolute risk may be exposed to potential side effects of a treatment for little or no therapeutic benefit.
The decision to treat or monitor without treatment should be based on patient global CV risk. Low-risk patients have a lower-chance of gaining benefit from treatment. These patients should be given lower priority for treatment when resources are limited.
President of the Egyptian Hypertension Society
M. Mohsen Ibrahim, MD
Prof. of Cardiology- Cairo University
References and Suggested Readings
G. Diagnostic evaluation of people with hypertension in low income country: cohort study of “essential” method of risk stratification. BMJ. 2008 Sep 19;337:a1387
- Paul S. Mueller. Clinic-based BP Measurement is Inaccurate for Diagnosing Hypertension. Journal Watch General Medicine August 11, 2011.
- Bui Q. Blood pressure treatment targets for uncomplicated hypertension. Am Fam Physician. 2010;81(7):848.
- Myers MG, Godwin M, Dawes M, Kiss A, Tobe SW, Kaczorowski J. Measurement of blood pressure in the office: recognizing the problem and proposing the solution. Hypertension. 2010;55(2):195-200
- Hodgkinson J, Mant J, Martin U, Guo B, Hobbs FD, Deeks JJ, Heneghan C, Roberts N, McManus RJ. Relative effectiveness of clinic and home blood pressure monitoring compared with ambulatory blood pressure monitoring in diagnosis of hypertension: systematic review. BMJ. 2011;342:d3621.
- Padfield PL. Reduction of cardiovascular morbidity and mortality in the third world: the importance of accurate blood pressure measurement. Hypertension. 2010;56(6):1038-9.
President’s Message
(April 2024)
When to Initiate Drug Therapy on First Office Visit?
Mohsen Ibrahim, MD
Prof. of Cardiology – Cairo University
President of the Egyptian Hypertension Society
The decision to initiate drug therapy in a hypertensive patient should not be taken lightly. Pharmacologic therapy of hypertension is a lifelong therapy. Once initiated, drug treatment will continue indefinitely since there is no cure from established essential hypertension except in rare conditions such as few secondary forms, or after extensive myocardial or brain infarction or after development of Addison’s disease. Blood pressure is quite variable between visits and even during the same office visit, where in some individuals readings can vary by 20 or 30 mmHg. Therefore, in order to avoid over-diagnosis of hypertension and prescribe unnecessary medications, it is mandatory not to initiate drug therapy on first office visit except in the following conditions:
- Hypertensive emergency.
- Severe hypertension after excluding a panic attack.
- High blood pressure with target organ damage (TOD).
- Hypertensive Emergencies
In hypertensive emergencies, high blood pressure is complicated by life threatening and or impending rapid progressive vital organ damage. Examples include severe hypertension associated with acute pulmonary edema, congestive heart failure, acute coronary syndromes (myocardial infarction, unstable angina), acute aortic dissection, hypertensive encephalopathy, eclampsia, intracerebral hemorrhage, cerebral infarction, subarachnoid hemorrhage and acute renal failure. Hypertensive emergencies necessitate immediate hospitalization, continuous blood pressure monitoring parenteral antihypertensive medications.
- Very High Levels of blood pressure (> 210/120 mmHg)that persist after repeated blood pressure measurements over 30 minutes or more and after exclusion of a panic attack will require patient observations, administration of rapid orally active antihypertensive drug such as calcium antagonists and checking blood pressure over the next 24 hours. Many patients with panic attacks present to the emergency department with severe elevations of blood pressure sometimes exceeding 210/120 mmHg that subside spontaneously after relief of patients severe anxiety. Panic attacks are characterized by short periods of intense fear or discomfort that develops abruptly and reaches a peak within 10 minutes. Panic attacks are accompanied by somatic and cognitive symptoms which include; shortness of breath, dizziness, hyperventilation, palpitations, trembling, sweating, feeling of chocking, nausea, abdominal distension, numbness, chills, chest pain, fear of dying, fear of going crazy or doing something uncontrolled. Normotensive patients with panic disorder have episodically hypertensive blood pressure readings with an increased heart rate. These hemodynamic alternations appear to be secondary to their panic attacks. Despite these episodic hypertensive periods, the mean ambulatory blood pressure remains within the normotensive range. Treatment includes patient reassurance, administration of a rapidly acting minor tranquillizer and follow-up. These hypertensive episodes usually subside in 30 minutes, while blood pressure returns to normal without antihypertensive drugs. Patients usually have a history of chronic anxiety and depression. Panic attacks are liable to reoccurrence. Identification of triggering situation and long term administration of an SSRI (specific seroterion receptor inhibitor) e.g. citalopram or referral to psychiatrist may be necessary.
- Patients seen for the first time with high blood pressure (≥ 180/110 mmHg) are candidates for antihypertensive therapy on first office visit if they have TOD and high blood pressure persists on repeated measurements in the office over 30 minutes. TOD includes clinical or electrocardiographic evidence of left ventricular hypertrophy or myocardial ischemia, optic fundus changes (hypertensive retinopathy), carotid bruits, peripheral arterial disease and proteinuria. Detailed laboratory evaluation is recommended in this group including renal function tests, abdominal ultrasound, carotid and peripheral arterial duplex ultrasound. Patients are seen within two weeks after initiation of antihypertensive therapy. Combination therapy is recommended in this high risk group on first office visit.
In absence of TOD, white-coat or isolated office hypertension should be excluded as a cause for patient’s high blood pressure. Blood pressure readings in these patients rarely exceed 180/110 mmHg during office visits. Blood pressure measurement outside office or at home is within the normal range (<140/90 mmHg). Ambulatory 24-hours blood pressure monitoring is the sure way to exclude white-coat hypertension. In some patients, blood pressure drops after repeated office measurements, however, in a good proportion high office blood pressure readings persists.
The management of these patients includes lifestyle modification; dietary measures, limiting salt intake, correction of obesity and solving family, social and work conflicts. Reassurance, treatment of anxiety and follow-up is recommended. Some patients with white-coat hypertension develop persistent elevation of blood pressure; therefore, blood pressure monitoring and repeated home measurements are needed. All precautions should be taken to obtain accurate blood pressure readings. Attention to details and following guidelines is essential. The EHS outlined, in its recent 2014 guidelines, the details and different steps that should be followed before and during blood pressure measurement procedure. Diagnosis and follow-up of hypertensive depends on obtaining accurate numbers.
President’s Message (July 2024)
DEPRESSION AND HEART
- Mohsen Ibrahim, MD
Prof. of Cardiology – Cairo University
President of the Egyptian Hypertension Society
Psychic depression is a common co-morbidity among hypertensive and cardiac patients. At least a quarter of cardiac patients suffer from depression and adults with depression often develop heart disease. Unfortunately many heart specialists may not have the time or expertise to address depression.
Major depression affects 10-13% of medical out patients.
On the other hand the majority of patients with major depression present with somatic complaints. Primary care physicians fail to diagnose depression in up to 50% of their depressed patients. Physical symptoms are often the chief complaint in depressed patients.
The diagnosis of depression is based upon the presence of the following complaints nearly every day for two weeks: depressed mood most of the day, inability to experience pleasure in normally pleasurable acts (anhedonia), significant change of weight, insomnia or hypersomnia, psychomotor agitation or retardation, fatigue or loss of energy, feelings of worth less-ness or guilt, impaired concentration and recurring thoughts of death or suicide.Symptoms must cause impairment of functioning.
Depression has been proven to be a risk factor in cardiac disease that the American Heart Association has recommended that all cardiac patients
be screened for depression using simple screening questions. Healthy individuals who suffer from depression are at significantly increased risk of developing heart attacks and strokes later in life.
The combination of depression and heart disease tripled the risk of death from all causes and quadrupled the risk of dying from a heart attack or a stroke. In the first six months after a heart attack, a depressed person’s chances of dying are four times higher than a non-depressed person, even if they have the same heart damage. Depressive symptoms have been shown to increase risk of stroke mortality over a 29 year period.
The physiological derangements linking depression to the heart include high sympathetic tone, hypercortisolemia, elevated catecholomine levels, abnormal platelet activation and endothelial dysfunction. Sympathetic outflow is increased in depressed patients.
Corticotropin- releasing factor (CRF) is increased in cerebrospinal fluid of depressed patients. CRF increases the levels of corticosteroids which may tigger atherosclerosis. Arterial endothelial function is significantly impaired in the depressed patients.
Anatomic abnormalities are present in the structures of limbic system (amygdala, hypothalamus, septal nuclei, cingulate and hippocampus with reduction in volume of prefrontal cortex and hippocampus.
Treatment of depression is effective and includes medications, psychotherapy or both. The type of treatment recommended depends on the type of symptoms, the severity of symptoms and the patient’s personal preferences. Combined treatment with antidepressants and psychotherapy
is recommended as first line treatment for patients with severe major depressive disorder.
Anti-depressant drugs include selective serotonin reuptake inhibitors (SSRIs) which are the most commonly prescribed, selective serotonin norepinephrine reuptake inhibitors (ENRIs) and tricyclic antidepressants.
Examples of SSRIs are citalopram( depram) , escitalopram (cipralex), paroxetine ( seroxat), fluoxetine( Prozac), sertraline (modapex).
Exomples of SNRIs are venlafaxine (effexor) and desvenlafaxine ( pristiq) .
Examples of tricyclic which are less commonle used are tryptizole.
Paroxetine (seroxat) is more anxiolytic than the others, while sertraline (modapex) is more effective in panic disorders.
Side effects are common with the majority of these drugs, and include nausea, sexual dysfunction, weight gain, drowsiness and dry mouth. It is recommended to start with an SSRI medication and increase the dose to therapeutic maximum dose. If patient does not tolerate the medication or does not show clinical improvement in 2-4 weeks, switch to antidepressant from the same class or preferably from another class with a different mechanism of action.
SSRIs, sertraline (Modapex) and citalopram (Depram) are safe for patients with coronary heart disease (CHD), and are the first line antidepressants drugs for patients with CHD.
Prevention of depression is based upon social support, physical exercise and stress management.
There is a need to educate physicians and to establish a system to identify, treat and follow-up cardiac patients with depression.
President’s Message
(October 2024)
NEW ANTIHYPERTENSIVE DRUGS
- Mohsen Ibrahim, MD
Prof. of Cardiology – Cairo University
President of the Egyptian Hypertension Society
Failure to achieve adequate BP control, correct the underlying pathophysiologic processes and the need for continuous non- interrupted drug intake are major limitations of current antihypertensive drugs, in addition to their possible side effects. Therefore, the search and trial of new antihypertensive drugs seems reasonable. There are basically two therapeutic targets for the new drugs: vascular targets and endocrine targets. The chief vascular target is the nitric oxide (NO), soluble granulate cyclase (SGC) and cyclic guano-sine mono phosphate (cGMP) pathway. SGC stimulators promote cGMP production and vascular smooth muscle relaxation.
The main endocrine targets are the mineralocorticoid receptor antagonists and natriuretic peptide receptors. Spironolactone is the mineralocorticoid receptor antagonist and the most effective antihypertensive, although its BP lowering effect was predicted by plasma renin activity and the aldosterone-renin ratio.
Eplerenone seems to possess a better safety profile than spironolactone. Hyperkalemia is an adverse effect of mineralocorticoid receptor antagonists that should be carefully considered in patients treated with these drugs.
Anti-aldosterone drugs are currently recommended in patients with resistant hypertension. These drugs will be used more frequently in the future.
Amiloride is a distal tubular diuretic that inhibits the aldosterone sensitive epithelial sodium channels. It is an effective alternative therapy to spironolactone for resistant HTN.
The different natriuretic peptides secreted by human heart (ANP, BNP, CNP) interact with membrane- bound particulate guanylyl cyclase (PGC). Activated GC intensifies the intracellular concentration of intracellular massanger cGMP which contributes to the activation of protein kinase leading to vasodilation and natriuretic and diuretic effects.
Neprilysin (NEP) is a membrane bound endopeptidase which contributes to the breakdown of vasoactive peptides leading to vasodilation, enhanced diuretic action, natriuresis and reduced sympathetic activity. Sacubitril is NEP inhibitor. Combination of valsartan and NEP inhibitor prodrug sacubitril ( Entresto) was superior to ARBs in cardioprotection. Angiotensin receptor neprilysin inhibitor (ARNI)- Entreto improved outcomes in cardiac dysfunction. The use of sGC stimulator or the prevention of cGMP degradation by blocking cGMP- degradation enzymes diaestrases phospho dia PDEs- Riociguat is SGC stimulator used in the treatment of pulmonary HTN. Riociguat also ameliorates portal HTN and liver cirrhosis.
SGC stimulators have promising antifibrotic, antihypertophic and anti- inflammatory effects.
Non-steroidal mineralocorticoid receptor antagonists as dihydropyridines Ca channel antagonists (Finerenone) are in clinical trials.
Endothelin receptor antagonists (ERA):
Endothelin is the most potent vasoconstrictor. ERA are indicated in pulmonary arterial HTN. ERA (aprocitentan) reduced BP in resistant
HTN. It is a blocker of both endothelin and endothelin-B receptors. ERAs produce fluid retention
SGLT2 Inhibtors
Empagliflozin and dapagliflozin reduce BP in diabetic patients more on daytime BP and their efficacy is comparable to low dose thiazide diuretics. They have renal protective effects which are also present in non diabetic CKD patients.
The mechanisms of antihypertensive effects of SGLTz inhibitors include osmotic diuresis, weight loss, improved endothelial function and reduced arterial stiffnes. The risks associated with SGLTz inhibitors include genital and urinary infections, bone fractures and acute kidney injury.
In spite of these advances the prevalence of HTN is still rising and a large proportion of hypertensive patients are under controlled
President’s Message
(January 2025)
SPECIALIZED HYPERTENSION CLINICS
Mohsen Ibrahim, MD
Prof. of Cardiology, Cairo University, President of the Egyptian Hypertension Society
The need for specialized HTN clinics should be stressed. The correct diagnosis and proper treatment of hypertension depends upon knowledgeable and experienced physician. The proper technique for BP measurement and the decision to start life-long drug therapy can be achieved through specialized HTN clinics.
Forthermore, the management of HTN necessitates long term follow-up. In Egypt HTN is a common disease but unfortunately it is mishandled. Rates of awareness, treatment and control are low. Establishing, specialized HTN clinics in Ministry of Health and universities hospitals will help avoid over and under diagnosis of HTN and select the proper timing for life long drug therapy. HTN requires long term follow-up with continuous monitoring of BP. Patients education regarding a healthy life-style that help control BP namely correction of obesity, healthy diet low in salt and rich in fruits and vegetables, regular physical exercise, avoidance of tobacco, alcohol and emotional stress.
Doctors running the clinics should receive educational courses regarding the proper technique of BP measurement, clinical and laboratory evaluation of hypertensive patients, when and how to initiate drug therapy, how to improve patients compliance and to avoid interruption of treatment.
The list of antihypertensive drugs is rapidly growing. The drugs of first choice will depend upon patient age, severity of HTN, presence of other risk factors and target organ damage.
Clinics may provide additional diagnostic services such as ambulatory BP recording, ECG, echocardiography and biochemical laboratory.
Information obtained from these facilities will guide the physician regarding the presence of target organ damage and the possibility of secondary HTN and the urgency and type of drug therapy.
Data collected from the clinics can provide important epidemio logic information regarding patients demographic characteristics, prevalence of hypertensive complication, rates of awareness, treatment and BP control among patients visiting the clinics, reasons of failure of BP control if present and prevalence and type of secondary HTN.
Active steps in the establishments of the clinics:
- Contact directors of hospitals and health authorities
- Stressing the need for specialized HTN clinics, choice of space, staff, diagnostic facilities, paper work and possibly antihypertensive
- Develop training courses for doctors, nurses and pharmacists; stress the importance of accurate BP measurement, the need for repeated measurements, choice of necessary laboratory tests, whea, to initiate drug therapy on first office visit, factors influencing the choice of antihypertensive drugs, when to refer patients for more detailed laboratory evaluation, when and how to interpret
ambulatory 24 hours BP recording if indicated, what to do with patients having resistant or difficult to control HTN.
- Possibility of providing antihypertensive drugs from hospitals pharmacies free of
- Increase public awareness of the clinics through posters, flyers, newspapers and
- Improve rates of follow-up through phone or e-mail, contact by nurses and clinic
- Stress the special services offered by the clinics namely reaching correct diagnosis, ABPM, identify patients in need of drug therapy and management of difficult to treat and resistant
- Physicians motivation through regular performance evaluation, certificates of excellence and presentation of data in scientific meeting, and quarterly progress reports and possibly financial
Outcome and benefits of the clinics:
HTN is a common disease affecting one quarter of adult Egyptians and more than fifty percent of elderly subjects. It is a major risk factor for heart failure, renal failure, stroke, coronary artery disease and peripheral arterial disease. Unfortunately because of its silent nature it is frequently undiagnosed unless complications develop. Treatment and control of HTN is possible but it is lifelong. Control of HTN can prevent strokes, heart attacks, heart and renal failure.
Components of physicians and pharmacists education program
- Mechanisms of BP regulation
- Definition of HTN
- HTN comorbidities:
- Diabetes
- Dyslipidemia
- Obesity
- Psychic depression
- Chronic renal disease
- Techniques for accurate BP
- Laboratory evaluation of hypertensive
- When to initiate lifelong drug therapy, factors influencing the choice of drug therapy and how to improve patients compliance
- When to start drug therapy on first office visit?
- How to manage a patient with hypertensive complication? and resistant HTN?
President’s Message
(April 2025)
Prevention of Coronary Heart Disease
Mohsen Ibrahim, MD
Prof. of Cardiology – Cairo University
President of the Egyptian Hypertension Society
The following president message is a summary of a review I finished writing under the same title “Prevention of Coronary Heart disease (CHD)”.
CHD is a common disorder and possibly the main reason for cardiologist visits and a main cause of morbidity and mortality.
CHD include a range of clinical disorders from asymptomatic atherosclerosis and stable angina to acute coronary syndromes (unstable angina, NSTEMI, STEMI).
In USA and the UK mortality rates due to CHD is decreasing through lifestyle changes and drugs. While in developing countries there is an increasing trend in mortality
CHD prevention is possible and is cost effective. Half of adults have at least one cardiovascular risk factor which are mostly undiagnosed. Healthful life style habits that do not permit the appearance of risk factors is the preferred method for prevention of CHD.
The WHO reported that ischemic heart disease was responsible for approximately nine million deaths in 2016.
Smoking cessation is important and its beneficial effect appears early after stopping smoking. Smoking appears to contribute to the generation of atherosclerotic plaques.
Weight Reduction in obese and over weight subjects ( body mass index >25 kg/m2) through both dietary and lifestyle changes. Weight loss can improve lipid profile, reduce BP and improve glycemic control.
A realistic target of weight reduction is 5-10% weekly weight loss of original weight.
Pharmacologic treatment should be considered only after dietary advice, exercise and behavioral approaches have been started.
Dietary approaches
The vegetarians experienced significantly less ischemic heart disease mortality than the non- vegetarian: CHD death rate in the non-meat eaters was around 25 % lower than in the meat eaters. It is recommended to replace butter and hard margarine with polyunsaturated margarine and full fat with skimmed milk and eat more fish, fiber rich foods, fresh fruit and vegetables.
Coronary angiography showed significant overall regression of coronary atheroma in an experimental group with very low fat vegetarian diet.
Physical exercise
People who exercise adequately have a reduced risk of CHD. The minimum exercise required to improve fitness is brisk walking for at least 20 minutes twice a week. Benefit can be obtained from less vigorous exercise in older people.
Coping with psychic stress and depression
Depression significantly increases the risk of CHD. Combined treatment with antidepressants and psychotherapy is recommended as first line treatment for patients with severe major depressive disorder.
Selective serotonin reuptake inhibitors (SSRIs) are the most commonly prescribed antidepressants.
Drugs for primary prevention
Statins lower LDL-Cholesterol with clinical benefit for CHD mortality and for all-cause mortality. The level of LDL-C and the presence of CV risk factors determine the need for statins in primary prevention.
Aspirin (75-100 mg/day) is indicated in all patients with prior CV event and for primary prevention in patients 50 years or older and have high risk and in patients with diabetes mellitus, 40 years or older and have additional risk factors. New clinical trials suggest a reduced benefit of aspirin for preventing first CVD events.
Conclusion:
Prevention of CHD is possible and cost effective. Nationwide awareness programs addressing both public and medical community are needed. These include CV risk factors prevention and treatment. Healthy lifestyle is the core of the prevention program. Cessation smoking, body weight reduction in obese, physical exercise and a healthy diet are the cornerstone for CHD prevention in addition to treatment of cardiovascular risk factors.
President’s Message
(July 2025)
Depression and Heart
Mohsen Ibrahim, MD
Prof. of Cardiology – Cairo University
President of the Egyptian Hypertension Society
Psychic depression is a common co-morbidity among hypertensive and cardiac patients. At least a quarter of cardiac patients suffer from depression and adults with depression often develop heart disease. Unfortunately many heart specialists may not have the time or expertise to address depression.
Major depression affects 10-13% of medical out patients.
On the other hand the majority of patients with major depression present with somatic complaints. Primary care physicians fail to diagnose depression in up to 50% of their depressed patients. Physical symptoms are often the chief complaint in depressed patients.
The diagnosis of depression is based upon the presence of the following complaints nearly every day for two weeks: depressed mood most of the day, inability to experience pleasure in normally pleasurable acts (anhedonia), significant change of weight, insomnia or hypersomnia, psychomotor agitation or retardation, fatigue or loss of energy, feelings of worth less-ness or guilt, impaired concentration and recurring thoughts of death or suicide.Symptoms must cause impairment of functioning.
Depression has been proven to be a risk factor in cardiac disease that the American Heart Association has recommended that all cardiac patients be screened for depression using simple screening questions. Healthy individuals who suffer from depression are at significantly increased risk of developing heart attacks and strokes later in life.
The combination of depression and heart disease tripled the risk of death from all causes and quadrupled the risk of dying from a heart attack or a stroke. In the first six months after a heart attack, a depressed person’s chances of dying are four times higher than a non-depressed person, even if they have the same heart damage. Depressive symptoms have been shown to increase risk of stroke mortality over a 29 year period.
The physiological derangements linking depression to the heart include high sympathetic tone, hypercortisolemia, elevated catecholomine levels, abnormal platelet activation and endothelial dysfunction. Sympathetic outflow is increased in depressed patients.
Corticotropin- releasing factor (CRF) is increased in cerebrospinal fluid of depressed patients. CRF increases the levels of corticosteroids which may tigger atherosclerosis. Arterial endothelial function is significantly impaired in the depressed patients.
Anatomic abnormalities are present in the structures of limbic system (amygdala, hypothalamus, septal nuclei, cingulate and hippocampus with reduction in volume of prefrontal cortex and hippocampus.
Treatment of depression is effective and includes medications, psychotherapy or both. The type of treatment recommended depends on the type of symptoms, the severity of symptoms and the patient’s personal preferences. Combined treatment with antidepressants and psychotherapy is recommended as first line treatment for patients with severe major depressive disorder.
Anti-depressant drugs include selective serotonin reuptake inhibitors (SSRIs) which are the most commonly prescribed, selective serotonin norepinephrine reuptake inhibitors (ENRIs) and tricyclic antidepressants.
Examples of SSRIs are citalopram( depram) , escitalopram (cipralex), paroxetine ( seroxat), fluoxetine( Prozac), sertraline (modapex).
Exomples of SNRIs are venlafaxine (effexor) and desvenlafaxine ( pristiq) .
Examples of tricyclic which are less commonle used are tryptizole.
Paroxetine (seroxat) is more anxiolytic than the others, while sertraline (modapex) is more effective in panic disorders.
Side effects are common with the majority of these drugs, and include nausea, sexual dysfunction, weight gain, drowsiness and dry mouth. It is recommended to start with an SSRI medication and increase the dose to therapeutic maximum dose. If patient does not tolerate the medication or does not show clinical improvement in 2-4 weeks, switch to antidepressant from the same class or preferably from another class with a different mechanism of action.
SSRIs, sertraline (Modapex) and citalopram (Depram) are safe for patients with coronary heart disease (CHD), and are the first line antidepressants drugs for patients with CHD.
Prevention of depression is based upon social support, physical exercise and stress management.
There is a need to educate physicians and to establish a system to identify, treat and follow-up cardiac patients with depression.
President’s Message
(October 2025)
Blood Pressure Variability (BPV)
M. Mohsen Ibrahim, MD
Prof. of Cardiology – Cairo University
President of the Egyptian Hypertension Society
BP is characterized by fluctuation over 24 hours period and between different office visits. Increase in BPV is harmful being associated with the development and progression of cardiovascular and renal complications. BPV may occur during the same office and between different visits, during home or 24 hours ambulatory BP monitoring (ABPM).
There are four types of BPV which include very short term that is beat to beat, short term over 24 hours, mid-term day to day and long term visit to visit. All types of variability are associated with increased risk of cardiovascular events: BP falls during sleep by an average of 10-20% of day time values and rises during the early morning hours. Short term BP variations within 24 hours are secondary to autonomic nervous system changes, humeral and emotional factors. Assessment of BP variability within 24 hours period requires continuous BP recording.
The standard deviation of the mean systolic and diastolic arterial pressure values can be calculated, coefficient of variation is calculated by dividing the average SD by corresponding mean BP. Day to day BP variability is assessed by ABPM over consecutive 48 hours period.
Home BP measurements can monitor BP changes over several days.
All types of variability are associated with increased risk of cardiovascular events. Day to day home BP variability is predictive of CV prognosis.
The prognostic role of day to day home BPV and clinic within visit and visit to visit BP variability have a role in risk stratification.
Systolic BPV correlates with arterial stiffness which is related to aging and increasing systolic BP. Diastolic BPV is related to impaired autonomic function with increased sympathetic activity and endothelial dysfunction.
BPV decrease with the decrease in average BP induced by drug treatments. Long acting dihydropyridine calcium antagonists are the most promising drugs in this regard, reducing ambulatory, home and clinic BPV.
Clinical significance of BPV: BPV introduces uncertainty in assessing subjects BP status and might be useful in improving CV risk stratification and may be a target for treatment.
President’s Message
(January 2026)
Prevention of Hypertension
M. Mohsen Ibrahim, MD
Prof. of Cardiology – Cairo University
President of the Egyptian Hypertension Society
